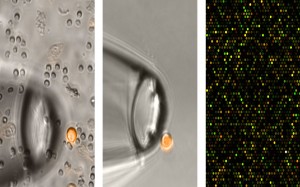
The pictures show the isolation of a breast cancer cell (small circle at left and center) and at right a section of their “molecular portrait.”
© Fraunhofer ITEM
How a cancer develops is often difficult to predict. The latest findings from Fraunhofer research help to better understand the course of the disease and to find the right personalized therapy for each patient.
The battle against cancer is a protracted fight for sufferers. Even when a tumor can be removed by surgery, the disease is far from defeated. Tumor cells spread through the bloodstream into other organs, where they can develop into new metastases. In order to render these disseminated cells harmless, the patient must undergo postoperative chemotherapy. New approaches to treatment, for breast cancer for instance, integrate molecular genetic findings to help choose the most effective drugs for each patient. Doctors examine the genetic “fingerprint” of the primary tumor; if e. g. expression of the gene HER2 is increased, the patient receives the drug Herceptin.
Even tumors with a size of 1 to 6 millimeters can spread
Researchers at the Fraunhofer Institute for Toxicology and Experimental Medicine ITEM have discovered something astounding. “The assumption that spreading cells have the same characteristics as the primary tumor is sometimes true, but far from always,” explains Prof. Christoph Klein, head of the ITEM project group “Personalized Tumor Therapy” in Regensburg. The scientist and his team found evidence that that cancer cells spread much earlier than was previously suspected. In the case of breast cancer, tumors are generally diagnosed at a size of 1-2 centimeters, but dissemination begins when the tumor is only between 1 and 6 millimeters. “At this stage of the disease, the primary tumor usually hasn’t even been detected yet. Consequently, its genetic profile also remains unknown at this point in time,” says Klein. Research using animal models has confirmed that the secondary tumors demonstrate different characteristics than an already palpable primary tumor. “It’s clear that cancer is an evolutionary process,” Klein explains. “Over the course of the disease, cells change.”
In order to ensure this translates into effective, targeted treatment, the researcher believes the focus at diagnosis needs to shift away from the primary tumor and towards the spreading cells. In this regard, the Regensburg project group works on methods for detecting cells using markers and then analyzing their molecular genetic profile. In a recently published study on melanoma for instance, the researchers could show that early-stage metastases were present in the sentinel lymph nodes; these provided insightful information about characteristic cell properties. The sentinel lymph node is the first lymph node in the tumor’s drainage area and therefore all disseminated tumor cells must pass through it. The study also showed a strong correlation between the number of metastatic cells in the sentinel lymph nodes and the risk of patient mortality. When this information is combined with known properties of the primary tumor, the patient’s prognosis can be reliably estimated.
In February, Prof. Klein was awarded the highly reputed German Cancer Prize for his research. He hopes to contribute to a better understanding of the dynamics of cancer and align that knowledge into better treatment strategies. “Our aim is to identify the right medications for a particular patient so as to prevent the actual formation of lethal metastases,” says Klein. For some patients, quite different measures than the highly toxic chemotherapy could potentially be of some help because, as the researchers have found, even cancer cells seem to be governed by Darwin’s survival of the fittest rule. Once they spread to other regions of the body, cells are subject to different selection pressure than they were at the point of formation. The good news is, most cells won’t survive, and therefore will never develop into secondary tumors.
Research News of the Frauenhofer-Gesellschaft Apr 30, 2014
